Excursion Week and Conflictive Decisions
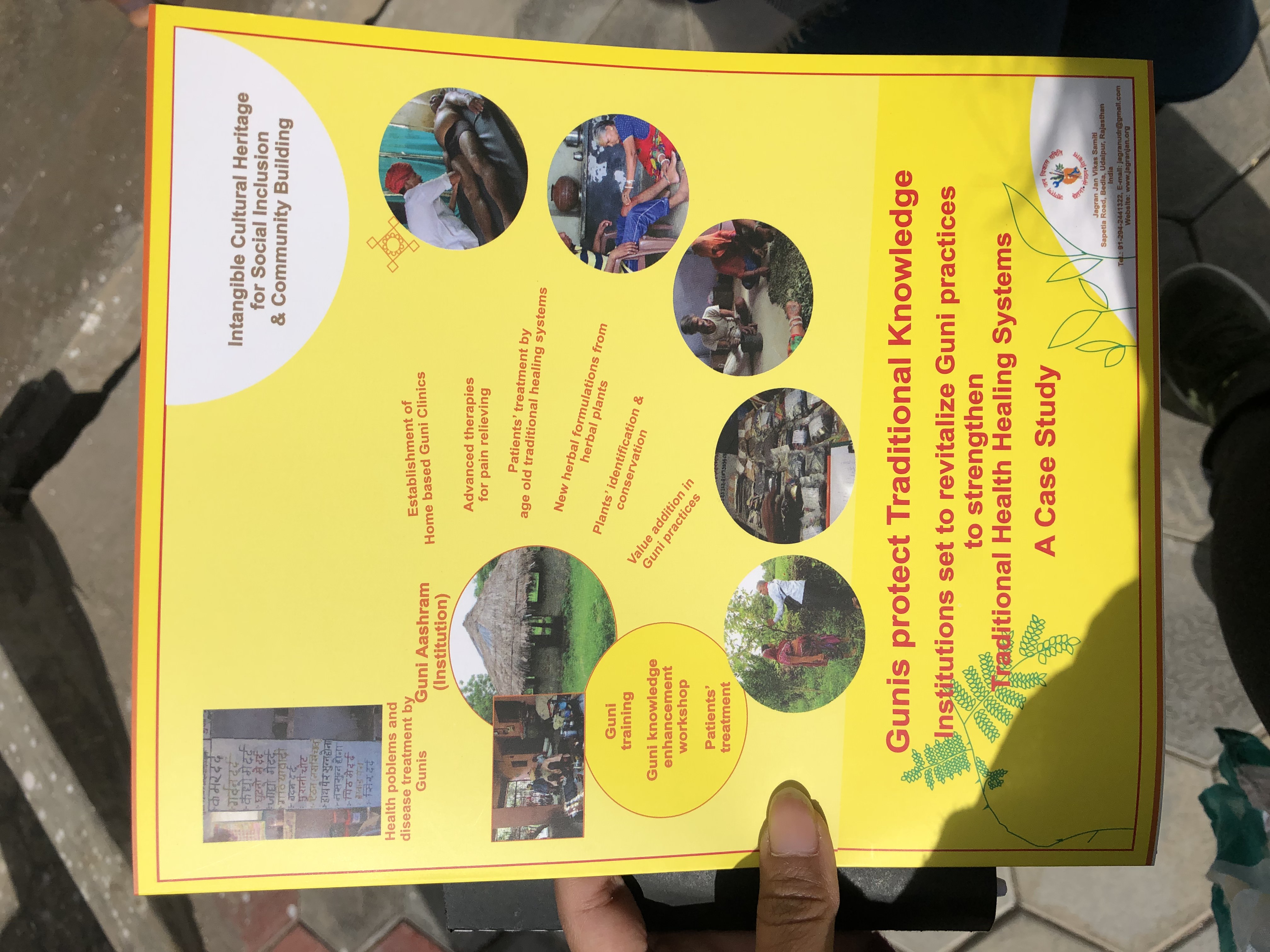
Week 3 was an excursion week for us and we traveled to Udaipur, Jaipur, and Agra while visiting different levels of the public healthcare system. We visited a Guni, a primary health center, a sub center, and a community healthcare center in rural and urban localities. At each location I entered, I deepened my understanding of how Indian patients seek and obtain care in addition to how healthcare providers perceive other providers depending on their practices and portions within hierarchies: social, medical, and otherwise. There were conflicting pieces of information I received from the different public health system components about what types of care are valid and should be used to treat patients. Ultimately, I had to make a decision on how to process the opinions I received from the healthcare professionals we learned from. At the different locations we went to, we talked with a traditional healer, a malnutrition treatment center operations manager and nutritionist, primary health center staff, a community health center doctor, an ASHA, JNM, AWW, and more healthcare workers who provide essential services to people in their communities. Some of the experts were telling us opinions that went against the labor of the other professionals that we’d met earlier in an indirect way. In other instances, healthcare experts would be more accepting and even supportive of others that don’t follow their mode of operations. The Ayurvedic doctor at the primary health center told our group that cross-referrals between allopathic and traditional doctors take place even though mutual institutional respect between the two forms of medicine is still lacking. The traditional healer (Guni) that we met said she didn’t feel unsupported by the government, especially she was still able to provide services, even on the way to the hospital or at the hospital, to her patients who needed ambulatory transportation to an allopathic center of care. All signs were pointing to positive perceptions, or at least improving opinions, between biomedical and traditional healers until we met with a doctor at a community health center. When asked about her opinion on Gunis, we had to explain to her what a Guni was and she firmly pushed back against their practices. She didn’t invalidate traditional medical practices even though she didn’t agree with them, but she said that they shouldn’t be practiced alongside allopathic medicine. In an ideal world, I would imagine that both allopathic and traditional healers could respect, learn from, and direct patients toward each other with patient wellness as the priority. The two types of medicine may be as separate as they are due to the presence of healthy skepticism toward each other, but both a willful and unintentional lack of knowledge about each other can exacerbate the divide and cloud perspectives with ideas of superiority and dominance. I don’t exclusively attribute the ignorance of other helpful medical systems to individual healthcare practitioners. The way medical professionals are officially and informally trained by academic instruction and generational knowledge largely impacts their understanding of, and thus interaction with, alternative forms of care. At the end of the excursion, I had to decide how to embrace the teachings I’d received throughout the week. I took into account what I’d previously thought about the distinctions between allopathy and traditional medicine and what I’d seen that blurred the distinguishing boundaries. My final decision was to appreciate the various forms of medicine I’d observed for their efficacy and applicability to different ailments. Going against my own pre-conceived notions about the irrefutable superiority of biomedicine through a Western lens, I chose to intentionally process what I experiences and understand that there are benefits to be earned from validating traditional, multi-generational practices, which can easily co-exist with Western medicine.